Volume 18, Issue 3 (May-Jun 2024)
mljgoums 2024, 18(3): 1-3 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kothari D R, Dutt N, Prajapati P, Garg P, Patel M. Analysis of broncho alveolar lavage adenosine deaminase assay in patients with clinically diagnosed pulmonary tuberculosis. mljgoums 2024; 18 (3) :1-3
URL: http://mlj.goums.ac.ir/article-1-1612-en.html
URL: http://mlj.goums.ac.ir/article-1-1612-en.html
1- Department of Respiratory Medicine, Narendra Modi Medical College, Maninagar, Ahmedabad, India
2- NHL Municipal Medical College, Paldi, Ahmedabad, India ,shishugarg@yahoo.com
2- NHL Municipal Medical College, Paldi, Ahmedabad, India ,
Full-Text [PDF 295 kb]
(577 Downloads)
| Abstract (HTML) (1875 Views)
Full-Text: (353 Views)
Introduction
Presently, tuberculosis (TB) is a major health problem globally. It is one of the common causes of death (1). The clinical features of TB are highly variable and depend upon the affected organ, ranging from asymptomatic non-specific complaints to respiratory failure. Many times, the symptom pattern mimics other pulmonary diseases. Radiographically, pulmonary TB (PTB) presents with different patterns on chest radiographs (2). The gold standard method for the diagnosis of TB is detecting the growth of Mycobacterium on smear and culture of bacilli in specimens like sputum, gastric lavage, bronchial washing, or lung tissue, or confirmed with other biochemical tests and DNA probes. The polymerase chain reaction (PCR) is a rapid, reliable, and highly specific method for the diagnosis of PTB. In smear-negative patients, the anti-TB treatment is delayed until results are available. Cartridge based nucleic acid amplification test (CBNAAT), Truenat MTB-RIF assay (TRUNAAT) and line probe assay (LPA) have considerably shortened the time for identification of mycobacterium and thereby helpful in initiating the treatment, but sometimes results may be delayed in addition to being very costly (3).
Adenosine deaminase (ADA) is considered a useful marker for the diagnosis of TB in various body fluids, and treatment is started accordingly. ADA is an enzyme produced from lymphocytes and involved in purine metabolism. It catalyzes the irreversible deamination of deoxyadenosine and adenosine to deoxyinosine and inosine, respectively, and is an indicator of active cellular immunity and T lymphocyte activity. There are two molecular forms, ADA1 and ADA2. ADA1 is found in most body cells, while ADA2 is found predominantly in the human plasma and serum. ADA activity is elevated in the sera of patients with hepatic diseases, hematological malignancies, and infectious diseases. Levels of ADA increase in TB because of stimulation of T cells by mycobacterial antigen. ADA levels in pleural fluid show good diagnostic accuracy in the diagnosis of TB pleural effusion since its levels are considerably elevated in patients with TB pleural effusion (4). To our knowledge, a few studies (5,6) have evaluated BAL ADA activity for the diagnosis of TB, and the results are variable. The aim of this study was to find out the effectiveness of BAL ADA in the diagnosis of PTB in sputum smear-negative patients.
Methods
We enrolled 40 patients, aged > 18 years, with an abnormal chest radiograph suggestive of PTB and negative for acid-fast bacilli smear examination even after induction of sputum with 3% normal saline from September 2021 to August 2022 after receiving approval from IRB Patients with bleeding tendency, respiratory failure, and HIV/HBsAg reactive status were excluded from the study. Written consent was obtained from all patients before undergoing study and bronchoscopy. Bronchoscopy was done using Olympus BF-1TQ170 bronchoscope. During the procedure, 10cc syringe with 9cc normal saline and 1 cc air was instilled through the bronchoscope, aspirated back, and collected in an infant mucus extractor. This was done a total of 3 times with most affected lobes and segments and stored at room temperature. BAL samples were sent for routine and microscopic examination, ADA, culture, and sensitivity for acid fast bacilli (AFB) and pyogenic organisms, cytology and CBNAAT examination.
ADA was measured by using the Quantitative Enzymatic principle in an automated machine. The laboratory turnaround time for BAL ADA is 45 minutes. As per case record form data was entered and analyzed. Follow-up was done for 6 to 9 months. Out of 40 patients, 11 patients were diagnosed with diseases other than TB; the remaining 29 patients were enrolled in the study. We had started anti-Koch’s therapy (AKT) in 29 patients. For the efficacy of BAL ADA, we considered sensitivity as an effective marker, and the formula for the Net Sensitivity of the parallel test was used. For that, an individual sensitivity of BAL ADA and BAL CBNAAT was done. For BAL ADA patients who improved after 6 months of AKT and BAL ADA>4 IU/L were considered as true positives, while patients who were not improved after 6 months of AKT and BAL ADA<4 were considered as true negatives. Patients whose BAL ADA >4 but did not improve on 6 months of AKT were considered as false positives and patients who improved with 6 months of AKT and BAL ADA < 4 were considered as false negatives.
For BAL CBNAAT, patients who improved after 6 months of AKT and BAL CBNAAT MTB detected were considered true positives, while patients who did not improve after 6 months of AKT and BAL CBNAAT MTB not detected were considered true negatives. Patients whose BAL CBNAAT MTB detected but did not improve on 6 months of AKT were considered false positives, and patients who improved with 6 months of AKT and BAL CBNAAT MTB not detected were considered false negatives. Statistical analysis was done using EPI INFO 7 software.
Results
Out of 40 patients, 29 were diagnosed with PTB, 11 patients with malignancy, and the remaining with miscellaneous diseases. Further analyses were done on data of the 29 patients who had PTB.
The mean age of the 29 subjects who were clinically diagnosed as having sputum-negative PTB was 36.8 years; out of them, 15 were male and 14 were female patients, with a mean duration of symptoms of 38.6 days. Chest radiographs showed that 23 patients had alveolar infiltrates, 5 had interstitial infiltrates, and one patient had a soft tissue opacity (Table 1).
BAL ADA Value:
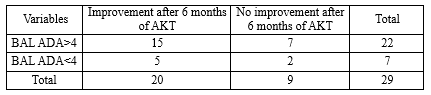
Out of 29 patients, 22 had a BAL ADA value > 4, while seven patients had < 4 BAL ADA value. All 29 patients were started on AKT treatment (Table 2).
Outcome of patients after 6 months of AKT treatment:
Out of 29 patients, 21 had BAL ADA 4.81±1.68, for whom AKT treatment was started and cured, while four patients with BAL ADA 4.50±2.86 did not improve and four patients with BAL ADA 6.52±1.16 whose AKT treatment is ongoing at present, clinically improved (Table 3).
Association of BAL CBNAAT with outcome:
Table 4 shows sensitivity of CBNAAT on BAL specimens in study patients. Out of 29 patients MTB was detected in 22 patients in CBNAAT test out of these 16 patients improved after anti tuberculosis treatment while 6 patients did not improve, in 7 patients MTB was not detected in BAL CBNAAT out of which 4 patients improved after giving AKT while 3 did not improve. Sensitivity of CBNAAT test in BAL specimens in this study is 80%.
When both CBNAAT and ADA tests were applied simultaneously on BAL specimens, the combined sensitivity turned out to be 95%.
Discussion
In TB, mycobacterial antigens stimulate T-cell lymphocytes, which raises the level of ADA enzymes. Raised ADA activity in patients with TB helps in the diagnosis of PTB as well as in extra pulmonary tuberculosis (EPTB) (6-9). The laboratory method for measuring ADA in BAL fluid is quite simple and inexpensive, so it can be done in laboratories with limited resources. In this study, the sensitivity of BAL ADA in association with the outcome was 75%, and the sensitivity of BAL CBNAAT with the outcome was 80%. When we applied a formula for combined sensitivity for a parallel test, it was 95%. Here, the outcome has two arms; one arm includes those patients on AKT and cured, while the second arm includes those patients with restarted AKT or ongoing AKT. In comparison to BAL CBNAAT, which is the gold standard test BAL ADA sensitivity is only 5% less. Also, we observed that two patients with BAL CBNAAT were not detected, but BAL ADA was > 4, and both were cured after AKT treatment.
Orphanidou and colleagues (6) compared lysozyme and ADA levels of BAL in sputum smear-negative but clinically diagnosed patients with PTB and respiratory diseases other than TB. This study suggests there is no statistically significant difference in lysozyme level, but the ADA level is significantly higher in sputum-negative PTB patients. In a study by Kayacan and co-workers (5), ADA level in BAL fluids of patients with PTB, non-TB respiratory disease patients, and controls was 3.1±2 IU/L, 0.4±0.5 IU/L, and 0.2±0.4 IU/L, respectively, (P<0.001). In a study done by Kubota et al. (10) the mean ADA level in BAL fluid of patients with sarcoidosis, miliary TB, idiopathic interstitial pneumonia, and control group was 1.06±0.99 IU/L, 5.02±3.75 IU/L, 0.21±0.43 IU/L, and 0.3±0.51 IU/L, respectively, and ADA level in BAL fluid of patients with miliary TB was significantly higher than that of other groups of respiratory disease (P<0.01).
BAL ADA value may differ from one race to another and also from one country to another (10). ADA level in BAL fluid of sputum smear-negative clinically diagnosed patients is significantly higher than in other respiratory conditions. Studies with a larger sample size are recommended for the sensitivity and specificity of BAL ADA.
Conclusion
We conclude that the sensitivity of BAL ADA with the outcome was 75% whereas in the case of BAL CBNAAT it was 80%. When we combined sensitivity for the parallel test, it came to 95%. So, we can conclude that BAL ADA is a very useful test in the diagnosis of PTB when a sputum smear for AFB is negative, but the patient clinically has TB.
Acknowledgement
We acknowledge and are grateful to all the patients who contributed to the collection of the data for this study. We are also thankful to Dr. Dipti Shah (Dean and Chairperson of MDRU), Dr. Nilesh Dutt (Professor and Head, Department of TB and Chest), and AMC MET Medical College, Ahmedabad, India.
Funding sources
NIL
Ethical statement
Ethical permission was received from the institutional review board AMC MET Medical College, Maninagar Ahmadabad, Gujarat.
Conflicts of interest
There is no conflict of interest.
Author contributions
Deep Kothari, Palak Prajapati, Mamta Patel and Pankaj Garg contributed to the conceptualization, data curation, formal analysis, investigation, methodology, resources, supervision, validation, writing (original draft), and writing (review and editing). Deep Kothari, Palak Prajapati, Mamta Patel and Pankaj Garg contributed to conceptualization, data curation, formal analysis, investigation, writing (original draft), and writing (review and editing). Deep Kothari, Palak Prajapati, Mamta Patel, Pankaj Garg and Nilesh Dutt contributed to the methodology, resources, supervision, validation, and writing (review and editing Deep Kothari, Palak Prajapati, Mamta Patel, Pankaj Garg and Nilesh Dutt contributed to the formal analysis, investigation, writing (original draft), and writing (review and editing). All the authors read and approved the final manuscript.
Presently, tuberculosis (TB) is a major health problem globally. It is one of the common causes of death (1). The clinical features of TB are highly variable and depend upon the affected organ, ranging from asymptomatic non-specific complaints to respiratory failure. Many times, the symptom pattern mimics other pulmonary diseases. Radiographically, pulmonary TB (PTB) presents with different patterns on chest radiographs (2). The gold standard method for the diagnosis of TB is detecting the growth of Mycobacterium on smear and culture of bacilli in specimens like sputum, gastric lavage, bronchial washing, or lung tissue, or confirmed with other biochemical tests and DNA probes. The polymerase chain reaction (PCR) is a rapid, reliable, and highly specific method for the diagnosis of PTB. In smear-negative patients, the anti-TB treatment is delayed until results are available. Cartridge based nucleic acid amplification test (CBNAAT), Truenat MTB-RIF assay (TRUNAAT) and line probe assay (LPA) have considerably shortened the time for identification of mycobacterium and thereby helpful in initiating the treatment, but sometimes results may be delayed in addition to being very costly (3).
Adenosine deaminase (ADA) is considered a useful marker for the diagnosis of TB in various body fluids, and treatment is started accordingly. ADA is an enzyme produced from lymphocytes and involved in purine metabolism. It catalyzes the irreversible deamination of deoxyadenosine and adenosine to deoxyinosine and inosine, respectively, and is an indicator of active cellular immunity and T lymphocyte activity. There are two molecular forms, ADA1 and ADA2. ADA1 is found in most body cells, while ADA2 is found predominantly in the human plasma and serum. ADA activity is elevated in the sera of patients with hepatic diseases, hematological malignancies, and infectious diseases. Levels of ADA increase in TB because of stimulation of T cells by mycobacterial antigen. ADA levels in pleural fluid show good diagnostic accuracy in the diagnosis of TB pleural effusion since its levels are considerably elevated in patients with TB pleural effusion (4). To our knowledge, a few studies (5,6) have evaluated BAL ADA activity for the diagnosis of TB, and the results are variable. The aim of this study was to find out the effectiveness of BAL ADA in the diagnosis of PTB in sputum smear-negative patients.
Methods
We enrolled 40 patients, aged > 18 years, with an abnormal chest radiograph suggestive of PTB and negative for acid-fast bacilli smear examination even after induction of sputum with 3% normal saline from September 2021 to August 2022 after receiving approval from IRB Patients with bleeding tendency, respiratory failure, and HIV/HBsAg reactive status were excluded from the study. Written consent was obtained from all patients before undergoing study and bronchoscopy. Bronchoscopy was done using Olympus BF-1TQ170 bronchoscope. During the procedure, 10cc syringe with 9cc normal saline and 1 cc air was instilled through the bronchoscope, aspirated back, and collected in an infant mucus extractor. This was done a total of 3 times with most affected lobes and segments and stored at room temperature. BAL samples were sent for routine and microscopic examination, ADA, culture, and sensitivity for acid fast bacilli (AFB) and pyogenic organisms, cytology and CBNAAT examination.
ADA was measured by using the Quantitative Enzymatic principle in an automated machine. The laboratory turnaround time for BAL ADA is 45 minutes. As per case record form data was entered and analyzed. Follow-up was done for 6 to 9 months. Out of 40 patients, 11 patients were diagnosed with diseases other than TB; the remaining 29 patients were enrolled in the study. We had started anti-Koch’s therapy (AKT) in 29 patients. For the efficacy of BAL ADA, we considered sensitivity as an effective marker, and the formula for the Net Sensitivity of the parallel test was used. For that, an individual sensitivity of BAL ADA and BAL CBNAAT was done. For BAL ADA patients who improved after 6 months of AKT and BAL ADA>4 IU/L were considered as true positives, while patients who were not improved after 6 months of AKT and BAL ADA<4 were considered as true negatives. Patients whose BAL ADA >4 but did not improve on 6 months of AKT were considered as false positives and patients who improved with 6 months of AKT and BAL ADA < 4 were considered as false negatives.
For BAL CBNAAT, patients who improved after 6 months of AKT and BAL CBNAAT MTB detected were considered true positives, while patients who did not improve after 6 months of AKT and BAL CBNAAT MTB not detected were considered true negatives. Patients whose BAL CBNAAT MTB detected but did not improve on 6 months of AKT were considered false positives, and patients who improved with 6 months of AKT and BAL CBNAAT MTB not detected were considered false negatives. Statistical analysis was done using EPI INFO 7 software.
Results
Out of 40 patients, 29 were diagnosed with PTB, 11 patients with malignancy, and the remaining with miscellaneous diseases. Further analyses were done on data of the 29 patients who had PTB.
The mean age of the 29 subjects who were clinically diagnosed as having sputum-negative PTB was 36.8 years; out of them, 15 were male and 14 were female patients, with a mean duration of symptoms of 38.6 days. Chest radiographs showed that 23 patients had alveolar infiltrates, 5 had interstitial infiltrates, and one patient had a soft tissue opacity (Table 1).
BAL ADA Value:
Out of 29 patients, 22 had a BAL ADA value > 4, while seven patients had < 4 BAL ADA value. All 29 patients were started on AKT treatment (Table 2).
Outcome of patients after 6 months of AKT treatment:
Out of 29 patients, 21 had BAL ADA 4.81±1.68, for whom AKT treatment was started and cured, while four patients with BAL ADA 4.50±2.86 did not improve and four patients with BAL ADA 6.52±1.16 whose AKT treatment is ongoing at present, clinically improved (Table 3).
|
Table 1. Patient’s characteristics
 |
|
Table 2. Association of BAL ADA with outcome
 |
|
Table 3. Outcome of patients after 6 months of AKT treatment
.PNG) |
Table 4 shows sensitivity of CBNAAT on BAL specimens in study patients. Out of 29 patients MTB was detected in 22 patients in CBNAAT test out of these 16 patients improved after anti tuberculosis treatment while 6 patients did not improve, in 7 patients MTB was not detected in BAL CBNAAT out of which 4 patients improved after giving AKT while 3 did not improve. Sensitivity of CBNAAT test in BAL specimens in this study is 80%.
When both CBNAAT and ADA tests were applied simultaneously on BAL specimens, the combined sensitivity turned out to be 95%.
|
Table 4. Association BAL CBNAAT with outcome
 |
Discussion
In TB, mycobacterial antigens stimulate T-cell lymphocytes, which raises the level of ADA enzymes. Raised ADA activity in patients with TB helps in the diagnosis of PTB as well as in extra pulmonary tuberculosis (EPTB) (6-9). The laboratory method for measuring ADA in BAL fluid is quite simple and inexpensive, so it can be done in laboratories with limited resources. In this study, the sensitivity of BAL ADA in association with the outcome was 75%, and the sensitivity of BAL CBNAAT with the outcome was 80%. When we applied a formula for combined sensitivity for a parallel test, it was 95%. Here, the outcome has two arms; one arm includes those patients on AKT and cured, while the second arm includes those patients with restarted AKT or ongoing AKT. In comparison to BAL CBNAAT, which is the gold standard test BAL ADA sensitivity is only 5% less. Also, we observed that two patients with BAL CBNAAT were not detected, but BAL ADA was > 4, and both were cured after AKT treatment.
Orphanidou and colleagues (6) compared lysozyme and ADA levels of BAL in sputum smear-negative but clinically diagnosed patients with PTB and respiratory diseases other than TB. This study suggests there is no statistically significant difference in lysozyme level, but the ADA level is significantly higher in sputum-negative PTB patients. In a study by Kayacan and co-workers (5), ADA level in BAL fluids of patients with PTB, non-TB respiratory disease patients, and controls was 3.1±2 IU/L, 0.4±0.5 IU/L, and 0.2±0.4 IU/L, respectively, (P<0.001). In a study done by Kubota et al. (10) the mean ADA level in BAL fluid of patients with sarcoidosis, miliary TB, idiopathic interstitial pneumonia, and control group was 1.06±0.99 IU/L, 5.02±3.75 IU/L, 0.21±0.43 IU/L, and 0.3±0.51 IU/L, respectively, and ADA level in BAL fluid of patients with miliary TB was significantly higher than that of other groups of respiratory disease (P<0.01).
BAL ADA value may differ from one race to another and also from one country to another (10). ADA level in BAL fluid of sputum smear-negative clinically diagnosed patients is significantly higher than in other respiratory conditions. Studies with a larger sample size are recommended for the sensitivity and specificity of BAL ADA.
Conclusion
We conclude that the sensitivity of BAL ADA with the outcome was 75% whereas in the case of BAL CBNAAT it was 80%. When we combined sensitivity for the parallel test, it came to 95%. So, we can conclude that BAL ADA is a very useful test in the diagnosis of PTB when a sputum smear for AFB is negative, but the patient clinically has TB.
Acknowledgement
We acknowledge and are grateful to all the patients who contributed to the collection of the data for this study. We are also thankful to Dr. Dipti Shah (Dean and Chairperson of MDRU), Dr. Nilesh Dutt (Professor and Head, Department of TB and Chest), and AMC MET Medical College, Ahmedabad, India.
Funding sources
NIL
Ethical statement
Ethical permission was received from the institutional review board AMC MET Medical College, Maninagar Ahmadabad, Gujarat.
Conflicts of interest
There is no conflict of interest.
Author contributions
Deep Kothari, Palak Prajapati, Mamta Patel and Pankaj Garg contributed to the conceptualization, data curation, formal analysis, investigation, methodology, resources, supervision, validation, writing (original draft), and writing (review and editing). Deep Kothari, Palak Prajapati, Mamta Patel and Pankaj Garg contributed to conceptualization, data curation, formal analysis, investigation, writing (original draft), and writing (review and editing). Deep Kothari, Palak Prajapati, Mamta Patel, Pankaj Garg and Nilesh Dutt contributed to the methodology, resources, supervision, validation, and writing (review and editing Deep Kothari, Palak Prajapati, Mamta Patel, Pankaj Garg and Nilesh Dutt contributed to the formal analysis, investigation, writing (original draft), and writing (review and editing). All the authors read and approved the final manuscript.
Research Article: Research Article |
Subject:
bacteriology
Received: 2023/01/12 | Accepted: 2024/02/21 | Published: 2024/05/30 | ePublished: 2024/05/30
Received: 2023/01/12 | Accepted: 2024/02/21 | Published: 2024/05/30 | ePublished: 2024/05/30
References
1. Caramori G, Lasagna L, Casalini AG, Adcock IM, Casolari P, Contoli M, et al. Immune response to Mycobacterium tuberculosis infection in the parietal pleura of patients with tuberculous pleurisy. PLoS One. 2011; 6(7): e22637. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Jeong YJ, Lee KS. Pulmonary tuberculosis: Up-to-date imaging and management. AJR Am J Roentgenol. 2008; 191: 834-44. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Hallur V, Sharma M, Sethi S, et al. Development and evaluation of multiplex PCR in rapid diagnosis of abdominal tuberculosis. Diagnostic Microbiology and Infectious Disease. 2013; 76(1): 51-55. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Klimiuk J, Krenke R. Role of biomarkers in making the diagnosis of tuberculous pleurisy. Pneumonol Alergol Pol. 2011; 79(4): 288-297. [View at Publisher] [PMID] [Google Scholar]
5. Kayacan O, Karnak D, Delibalta M, Beder S, Karaca L, Tutkak H. Adenosine deaminase activity in bronchoalveolar lavage in Turkish patients with smear negative pulmonary tuberculosis. Respiratory Medicine. 2002; 96(7): 536-541. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Orphanidou D, Gaga M, Rasidakis A, Dimakou K, Toumbis M, Latsi P, et al. Tumour necrosis factor, interleukin-1 and adenosine deaminase in tuberculous pleural effusion. Respir Med. 1996; 90(2): 95-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Piras MA, Gakis C, Budroni M, Andreoni G. Adenosine deaminase activity in pleural effusions: an aid to differential diagnosis. British Medical
Journal. 1978; 2(6154): 1751-52. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Valdés L, San José E, Alvarez D, Sarandeses A, Pose A, Chomón B, Alvarez-Dobaño JM, Salgueiro M, et al. Diagnosis of tuberculous pleurisy using the biologic parameters adenosine deaminase, lysozyme, and interferon gamma. Chest. 1993; 103(2): 458-465. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Bueso JF, Hernando HV, Garcia-Buela JP, Juncal LD, Egana MTM, Martinez MCM. Diagnostic value of simultaneous determination of pleural adenosine deaminase and pleural lysozyme/serum lysozyme ratio in pleural effusions. Chest. 1988; 93(2): 303- 7. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Kubota M, Katagiri M, Yanase N, Soma K, Tomita T. Measurement of adenosine deaminase activity in bronchoalveolar lavage fluids as a tool for diagnosing miliary tuberculosis. Nihon KyobuShikkan Gakkai Zasshi. 1996; 34(2): 139-144. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Choi SH, Kim YS, Bae IG, et al. The possible role of cerebrospinal fluid adenosine deaminase activity in the diagnosis of tuberculous meningitis in adults. Clinical Neurology and Neurosurgery. 2002; 104(1): 10-15. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.